Building a Business Case for Medtech Transformation
The “R” in ROI
Good investments produce a good return.
If you buy a house as an investment property, you expect its value to increase. You expect to receive income from renting it. To understand the return, you also have to understand the costs. How much will you pay for the house? How much will you spend up front to make it a desirable rental? What are the maintenance costs? Mortgage interest? Taxes?
The return is made up of the benefits—rent, future profit on eventually reselling the house—minus the costs. You also need to account for the time value of money. Future benefits and costs are worth less than immediate ones. That’s why, if you borrow money to make this investment, you have to pay interest to the banker on the loan.
Putting all this together gives you the return on investment or ROI.
It’s helpful to think of digital transformation investments in the same way. There’s a cost to “build” the asset and a cost to run and maintain it. There are tangible benefits you anticipate. You make the investment because you want to improve some things. You want to increase revenues, or profits. You want to improve speed to market. You want to reduce costs. Or eliminate risks.
But you can’t always directly look up the current costs of doing business or precisely forecast revenue gains or risk reduction. That’s because the things you want to improve are often complex and there are usually some unknowns involved.
So, understanding the ROI of a transformation requires a bit of measurement and a bit of analysis. It’s worth the effort to do this, because having a good business case is important to making sure your strategy—the things you’re trying to improve—is a good strategy.
Building a medtech business case
How should you go about building the business case?
Medtech investments usually require senior management approval, so it’s important to articulate the why, what, and how in a clear and simple way.
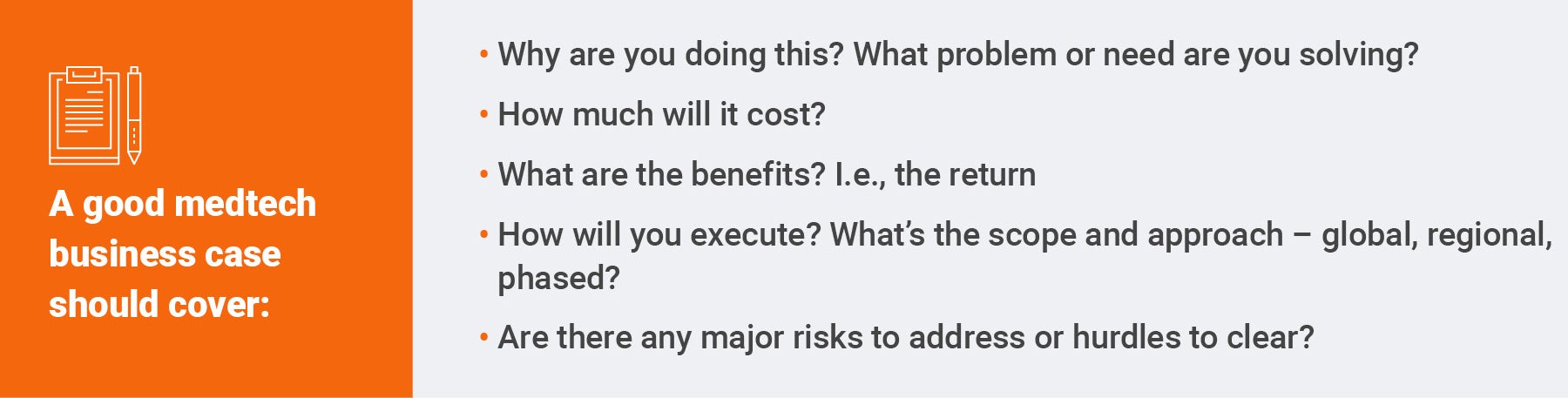
This can all fit on one page. And it should. It’s good to have more detail on each of these points—for example a timeline graphic, or who the partners and team will be—but these details should follow the crisp summary.
The business case will help explain to senior leadership why this investment is the right one versus alternatives. There’s always competition for budgets and resources. Your strategy must stand out and be clearly articulated to get funded. It’s often helpful to explain what options you looked at and what the decision criteria were. The decision criteria usually are heavily weighted to financial benefit.
Even though there’s some analysis required, building the business case doesn’t need to be overly complex. By understanding the current state—for example the cycle time of a key process, or hours taken to complete key steps, or excess external contractor costs incurred due to inefficiencies—you can easily estimate current costs in resources or dollars.
Having metrics or key performance indicators (KPIs) is important. These baselines tell you how you’re doing today, so that when you work on a digital transformation, you can verify the improvements. That’s a business benefit.
If you’re coming from very manual environments—not uncommon in medtech—you might not have KPIs or baselines. In this case, it’s often possible to estimate them using a sampling or interviewing approach. Sometimes even this isn’t feasible. In that case, using industry benchmarks as future targets is a good approach.
The same goes for revenue growth. It’s okay to use good estimates to ground the business case. For example, you can use the anticipated revenue for a new product launch to estimate the revenue benefit of getting it to market weeks or months faster.
The advantages of cloud-native software
Traditionally, on-premise software is replaced every five to seven years. That’s like buying a house you can never maintain and have to rebuild all the time.
There’s a big investment advantage to cloud-native software as a service (SaaS) in this respect. There’s only one physical version of the software. There are multiple yearly releases that add features. New features create new benefits—like having periodic kitchen upgrades without extra cost. That’s a significant benefit.
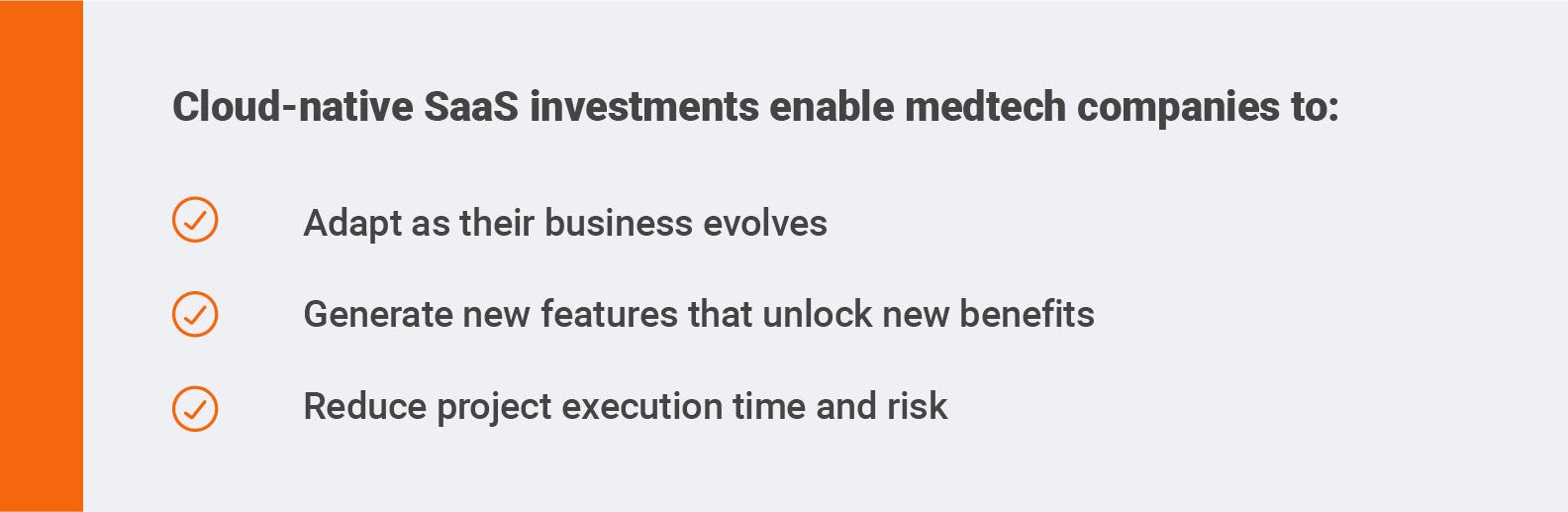
Cloud-native SaaS also reduces risk, because it doesn’t promote the accumulation of technical debt and process debt. As well, older on-premise software always has hidden costs, like infrastructure hosting and excess customization. The Veeva Vault Platform, in particular, also has built-in compliance. This is critical for medtech, and it reduces both risk and cost.
In this context, it’s important to understand the difference between cloud-hosted and cloud-native, multi-tenant SaaS. Partners who are not cloud-native may represent these as the same, but they’re not. Cloud-hosted software is a lot like on-premise software, except that you are renting the hosting and infrastructure rather than maintaining your own data centers. This is helpful because it’s complex and expensive for industry to run data centers, but cloud-hosted software generally still has multiple versions. So, it doesn’t solve the problem of technical debt accumulation and version management.
Good cloud-native SaaS adapts as the business evolves. Because there’s only one version of the software, all the changes are available with each periodic release. That helps ensure the things you wanted to fix—your business case—continue getting better. That’s also why cloud native SaaS is a better way of powering digital transformations. It has a predictable cost structure with accelerating capabilities.
With standard packaging configuration and minimal customization, it’s faster and easier to implement industry standard best practices. Standard configurations also minimize the common problem of time and cost overruns that result from excess complexity.
All together these advantages make up a sound investment that produces a good return.
How to think about risk in a medtech business case
Execution risk relates to what might go wrong in a project. Good project management methodology—and choosing the right kind of software—can mitigate execution risk.
What about underlying business risk?
Reducing compliance risk and business risk is often an investment rationale, but it can be tricky to “price” the risk. There aren’t actuarial tables that can quantify this kind of risk the way there are for car insurance or life insurance.
Every medtech manufacturing and quality leader plans to have zero recalls. Yet, recalls do happen. And when they happen, there’s a significant cost—both financial and reputational—to remediate them. The same applies to compliance fines.
Creating baselines can help. While of course you plan to have no recalls, if in fact you’ve had 2-4 recalls per year on average over the past five years, you can use that to baseline. Let’s imagine these are large class I product recalls with an average cost of $20 million to address. Now, your baseline recall cost is $60 million per year. If that’s the case, your controls need improvement, and you have the foundation of a business case. You could complete a similar analysis for compliance fines. If you’re concerned about controls but you haven’t had major issues, you can still look at comparables in the industry and estimate a cost of risk that way
Regardless, quantifying the cost of failure, either with your own data or with reference to comparables, helps make the case. It’s also important to note that compliance costs have risen over the past decade due to more complex supply chains, stricter regulatory requirements, and increased litigation.
In addition to pricing risks as best as you can, it’s also helpful to build out some story points. Have you had a lot of near misses? You can gather details by talking to the people who are running the operation and are experiencing the pain of bad processes, systems, or controls. These true horror stories about what went wrong, or almost went wrong, help bring the gravity of the problems to life for senior leaders, who are often removed from the day-to-day.
Distinguishing between hard and soft benefits
The difference between hard benefits and soft benefits is one of the most misunderstood aspects of defining business value—outside of CFOs and their teams. Since CFOs typically approve major investments, it’s important to understand and explain the benefits case in their language.
Businesses use two major “schedules” to measure their financial performance:
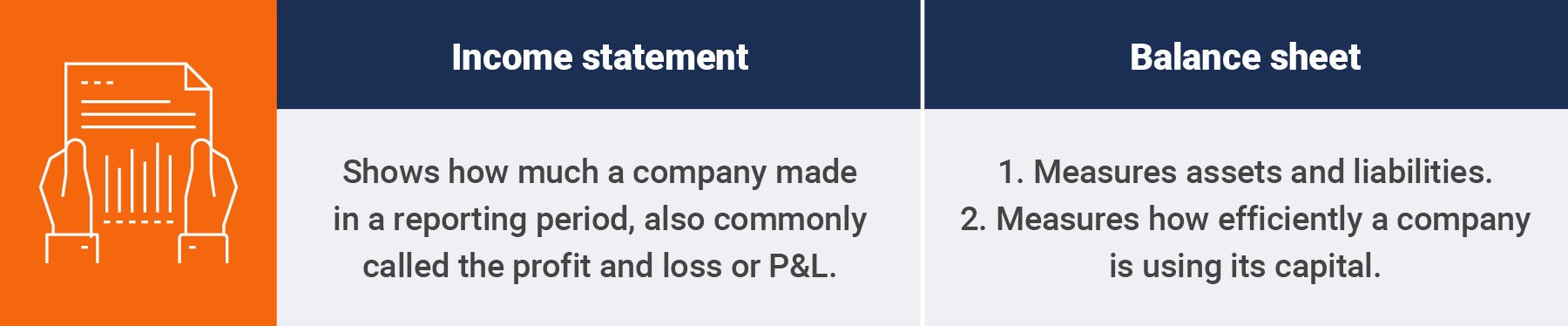
The income statement is made up of top line revenues, minus the cost of goods sold (cost to manufacture or service), minus sales general and administrative costs, minus taxes (and sometimes special items).
Top line revenues minus cost of goods sold is the gross margin, and the gross margin minus sales general and administrative costs is the net margin or operating margin.
The balance sheet consists of all the company’s long and short assets (including factories, cash, accounts receivable, intellectual property, etc.) and liabilities (including debt, accounts payable, etc.).
From a finance lens, hard benefits show up in the P&L, the balance sheet, or both. Soft benefits or avoidance benefits do not show up.
This means that a very strong financial business case will improve revenue or gross margins or net margins on the P&L. That is, we need more revenue or less cost—either cost of good sold or sales general and administrative costs. Or we need to improve asset utilization or reduce assets on the balance sheet to free up capital.
For most CFOs, being more efficient or improving the user experience does not equal a hard benefit, unless we are not physically improving revenues, costs, or asset utilization. Usually, these soft benefits or cost avoidance will not count towards return.
It’s still worthwhile quantifying soft benefits as well as we can and they are still a good story point, but hard benefits—especially P&L improvements in revenue or margins—rule in finance. That’s why wherever possible you should try to reframe soft benefits like “quality and regulatory team efficiency” as hard benefits like “faster change control reducing the cost of goods sold by qualifying more cost effective raw materials in our supply base”.
How to sustain medtech business value over the long term
Once you’ve defined your business case and received the investment, you’re all done, right?
In fact, that’s just the beginning.
Just like the metaphor of the house investment, once you have the funding and you buy the house, then someone lives in the house and gets the benefits of living there.
In the same way, when you planned a digital transformation project, you promised the business some new benefits, and when that project is complete, you have to measure the outcomes. That is how you live up to the promises you made and breathe life into the transformation strategy.
Doing this is difficult and requires some attention. Most medtech companies struggle in the value realization phases of a transformation, and there are several typical reasons for this:
- Projects are tiring and people want to “get back to normal” rather than embedding the improvements
- You are asking people to work in new ways—this change management is hard
- Despite your best efforts, you may not have captured the value or the baselines sufficiently
- There are often accountability gaps in who owns the outcomes. Who will drive the process to make sure that the organization delivers the benefits?
- New metrics can change performance incentives. Misaligned incentives encourage people to work in the old way or some tangential way
There are three key moments in the life of a transformation investment. In the house metaphor those are 1) when you decide to buy the house, 2) when you actually buy (or build it), and 3) when someone moves in and lives in it.
To sustain value, you still have to focus on the why, the what, and the how.
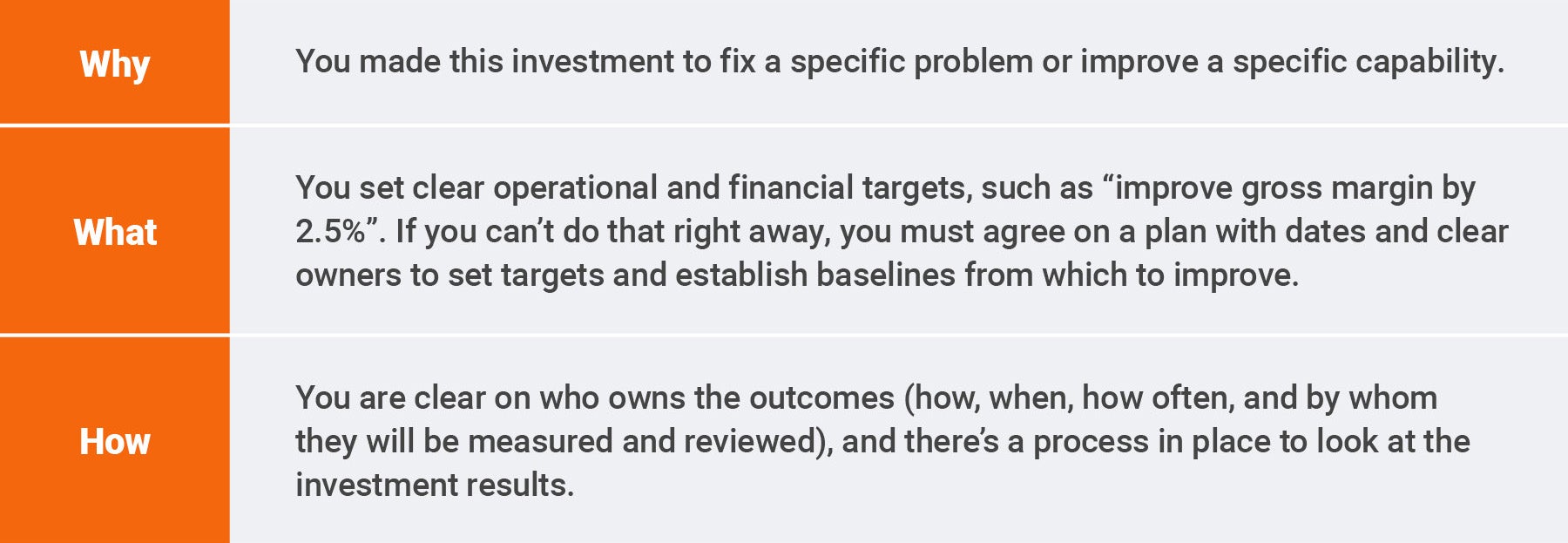
Finally, you need sponsorship and alignment. While CFOs are often tough on investment approvals—that’s their job after all—they are excellent sponsors to hold the organization accountable. The same goes for senior leaders in operations, sales, and HR. The right steering team or governance structure is key to making sure an investment delivers on the business value envisioned in the strategy.
Explore More:- Smith+Nephew: Unpacking the Critical Roles of Clinical and Medical Affairs [Article]
- LivaNova: Reducing Compliance Risk with Simplified Promotional Material Management [Video]
- Electronic Submissions are the Future of Medical Device Regulation – Why the Wait? [White Paper]
- Teleflex: Data-Driven Quality for Patient Safety and Rapid Resolution [Video]