Blog
5 Ways to Adapt Clinical Trial Oversight Processes for ICH GCP E6(R3) Compliance
Oct 22, 2025 | Pinar Bérénice Benét
Oct 22, 2025 | Pinar Bérénice Benét
Now that ICH GCP E6(R3) is in effect, sponsors face a heightened call for proactive, risk-based oversight strategies. Although this change may seem daunting, especially for sponsors who rely heavily on outsourcing, R3 also presents an opportunity to reevaluate and modernize existing processes.
Here are 5 ways sponsors can adapt their oversight plans to run effective and R3-compliant clinical trials:
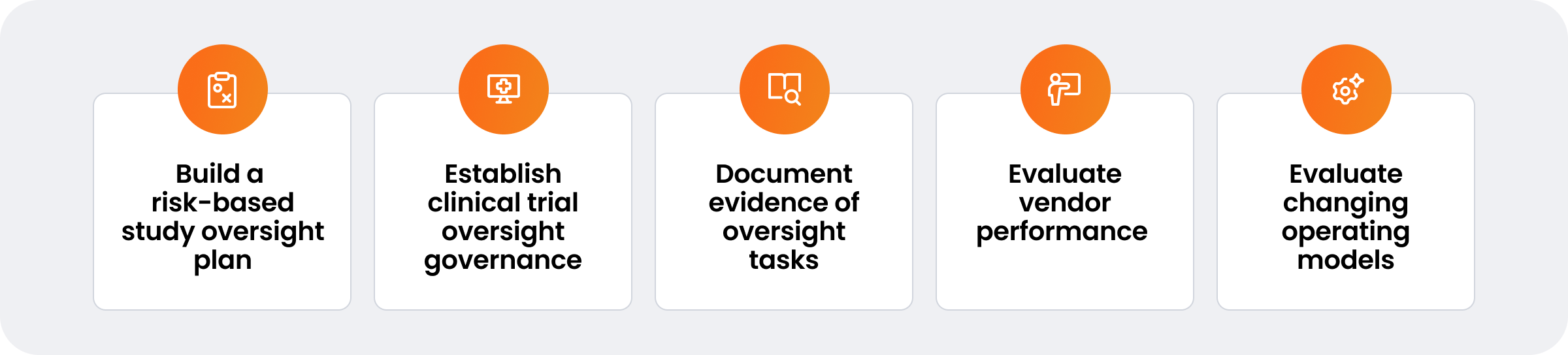
1. Build a risk-based study oversight plan
The first step in a comprehensive oversight plan is a clear definition of essential data and review parameters. Identify the specific set of data (essential records) that requires review. Determine the frequency of these reviews and assign responsibility to qualified personnel. Emphasize both the quantity and quality of resources, ensuring the team has adequate oversight experience and expertise.
Next, tailor the oversight strategy to the trial type, phase, and associated risks. This ensures that higher-risk areas and sites receive appropriate attention. As applicable, co-define acceptable ranges — previously referred to as quality tolerance limits — for in-scope activities with relevant CROs or sites. Continuously adapt oversight plans to emerging risks as they are identified.
Engage CROs early in the process to align on expectations and responsibilities. Determine how CROs will provide or transfer oversight data, such as issues, protocol deviations, documents, and associated audit trails, to the sponsor system in real-time.
Finally, develop KPIs to identify oversight issues. These may include metrics for study progress, deviations, monitoring visit report (MVR) timeliness, quality issues, and time taken to resolve issues. Document all actions taken to address findings, and ensure a contingency plan is in place to manage unforeseen issues during the trial.
2. Establish study oversight governance
Governance is a cornerstone of effective clinical trial oversight. It ensures that oversight issues are identified, addressed, and resolved systematically. Begin by establishing an oversight governance team that extends beyond the traditional study team. This might include representatives from clinical operations, data management, quality assurance, and regulatory affairs.
Next, create dedicated sponsor oversight roles. In addition to cross-functional governance, consider assigning study-level oversight responsibilities to an oversight manager or a study/trial operations manager.
Schedule regular oversight governance meetings to proactively manage potential challenges and adapt as needed. A well-structured agenda should include a review of study progress, trends, deviations, quality issues, and risk assessments. Always document the rationale behind each decision, data reviewed, and actions to reach desired outcomes.
3. Create and document evidence of oversight tasks, issue management, and study data reviews
Continuous data review and oversight tasks help maintain trial integrity. Best practices include:
- Distributing oversight tasks to specific study team members
- Reviewing CROs’ study operational data regularly, focusing on records that pose the highest risk to the trial
- Reviewing (or ensuring CROs review) site data regularly. This includes real-time tracking of site receipt and acknowledgement of safety letters, essential documents, and training
- Implementing solutions to retain institutional memory and digitize sponsor/CRO-site interactions, such as escalations tracked per site
- Documenting task completion in a centralized system, including deviations and communication logs
- Recording oversight issues and noting the specific data reviewed to inform decision-making
- Tracking evidence of oversight records using validated clinical trial technology to maintain data integrity, demonstrate regulatory compliance, create audit trails, and improve transparency
4. Evaluate CRO and vendor performance
Effective vendor oversight requires a structured evaluation process. Start by forming a cross-functional team with members from clinical operations, procurement, and quality assurance to lead vendor performance management.
Define clear, measurable KPIs for vendor performance—such as data quality, adherence to timelines, and regulatory compliance. Throughout the partnership, regularly review progress against these KPIs, document findings, and adjust plans as needed.
Establish a continuous feedback process with vendors to address performance gaps, implement improvement plans, and leverage insights from past evaluations to strengthen future collaborations.
5. Evaluate changing clinical operating models
With R3 now in effect, many sponsors are considering bringing systems and processes in-house to increase oversight. Begin with an activity split assessment to determine which activities should be executed internally versus managed by CROs. The split will vary by function and depend upon the sponsors risk tolerance, cost structure, and operational efficiency goals.
Transitions of this scale require a custom operating model that spans all relevant functions and serves as a go-to reference for post-transition operations. Sponsors should assess the potential challenges within each function to determine whether the current technology stack can support their target model.
Prioritize change management to help teams adapt to new systems and processes, ensuring smooth adoption and sustained performance.
Update internal business procedures to align with the new model, and establish a strong decision-making framework—typically a high-level executive steering group for major risks and a smaller transition oversight board to guide early-stage activities.
Learn why every sponsor needs a validated clinical trial oversight system for R3 compliance